Individual Outcomes
To a large degree, System Outcomes are a reflection of what is happening in the clinical relationships between the consumer and their care team as well as the consumer and their natural supports. When it comes to actual improvement for an individual, it is much more important to identify and work with Performance Measures that are meaningful to the consumer – thus the need for a more individualized performance measurement system.
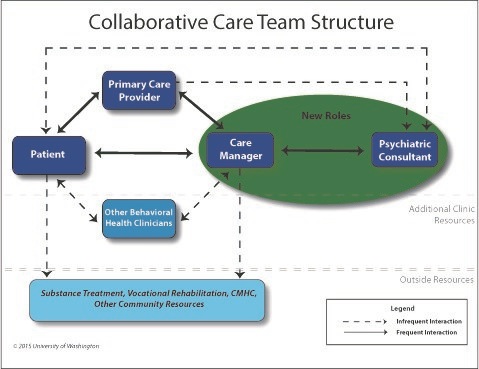
The University of Washington AIMS Center, among other groups, has pioneered a Collaborative Care model that represents an evidence-based approach to integrated care, which focuses on putting identifying measures that are important to the individual at the center of the care planning and delivery process. This model has been tested in more than 80 randomized controlled trials in the primary care clinic setting the US and abroad.
A rich treasure trove of material can be found at https://aims.uw.edu/collaborative-care.
In Washington State, this model has been implemented in Federally Qualified Health Centers and Rural Health Centers in every county based on the following principles:
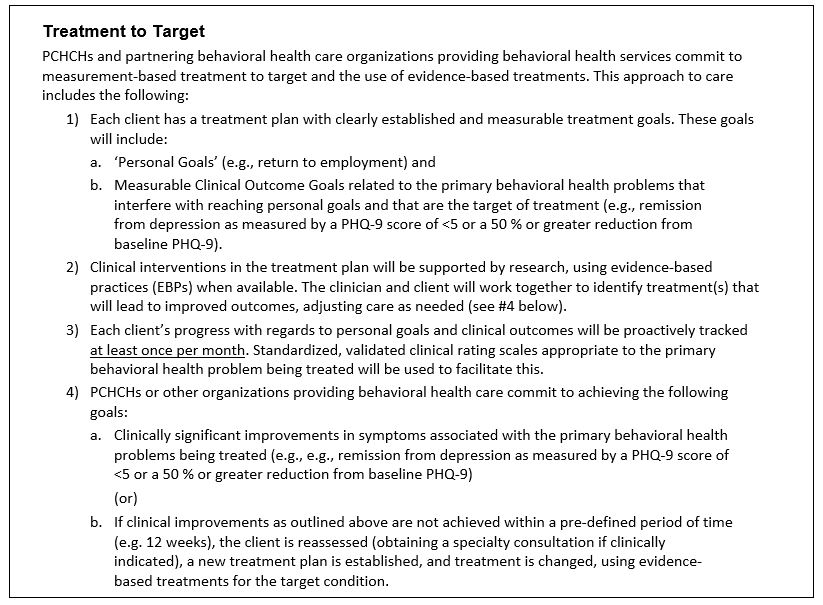
Treatment to Target: A key design element of this approach has been the use of Treatment to Target, which is described as follows:
The University of Washington AIMS Center, among other groups, has pioneered a Collaborative Care model that represents an evidence-based approach to integrated care, which focuses on putting identifying measures that are important to the individual at the center of the care planning and delivery process. This model has been tested in more than 80 randomized controlled trials in the primary care clinic setting the US and abroad.
A rich treasure trove of material can be found at https://aims.uw.edu/collaborative-care.
In Washington State, this model has been implemented in Federally Qualified Health Centers and Rural Health Centers in every county based on the following principles:
- All clients have a Person Centered Health Care Home (PCHCH) that is responsible for provision or coordination of preventive, acute, or chronic health care services, including behavioral health (mental health and substance use disorder) services.
- All clients have one problem list, one medication list, and one care plan that is shared by all providers including behavioral health providers. Progress on goals of care is systematically tracked and visible to clients and participating providers inside and outside the PCHCH.
Treatment to Target: A key design element of this approach has been the use of Treatment to Target, which is described as follows:

Outcomes-Based Care in Specialty Behavioral Health: In 2014, the mental health leadership at Oregon’s largest Medicaid Health Plan (Health Share of Oregon, began an Outcomes-Based Care program for the specialty mental health providers in the three counties in the Portland Oregon area. The program is, based on the AIMS Center Collaborative Care Model, is intended to test Outcomes-Based Care/Treatment to Target for the children, youth and adults that meet criteria for specialty behavioral health. This population is very similar to the Arizona RBHA target population.
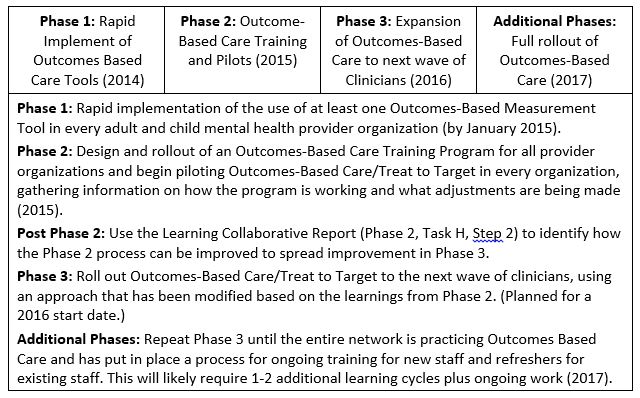
The program has been designed to roll out in multiple phases as illustrated by the table below.
The program has been designed to roll out in multiple phases as illustrated by the table below.

Implementing Outcomes-Based Care Tools: The leadership in the Portland Oregon system developed a set of important criteria for determining the tools that would be put on the Outcomes-Based Care Clinical Tool Menu. The criteria included the following:
Health Share of Oregon’s Clinical Tools Menu Criteria
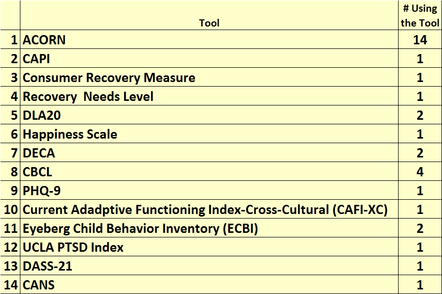
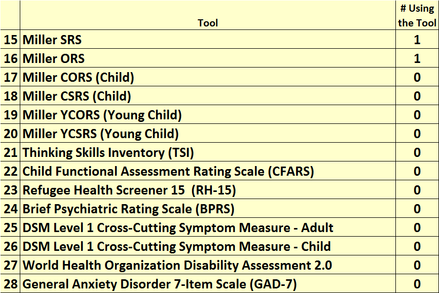
Health Share’s mental health leadership worked with the Center for Clinical Informatics (www.psychoutcomes.org) to evaluate clinical tools that were currently in use or might be relevant to the project. Together the researchers and a clinical workgroup developed a menu containing the tools listed below.
Health Share of Oregon’s Clinical Tools Menu Criteria
- The tool must measure a clinically relevant symptom, function or behavioral domain.
- The tool must use a scoring scale that supports the ability to do sequential measurement and has a track record for reliability and validity.
- The tool must help the client and clinician determine whether the client is making progress.
- The tool must be short and preferable self-reported by consumer/client when possible.
Health Share’s mental health leadership worked with the Center for Clinical Informatics (www.psychoutcomes.org) to evaluate clinical tools that were currently in use or might be relevant to the project. Together the researchers and a clinical workgroup developed a menu containing the tools listed below.
The Importance of Outcomes-Based Care at the Individual Client Level: This work along with similar projects at the Mental Health Center of Denver and the National Council for Behavioral Health is on the leading edge of Behavioral Health Performance and should be seriously considered by the RBHAs and Arizona’s Behavioral Health Providers. For more information on the Denver and National Council’s project, go to the following websites.
Mental Health Center of Denver Reaching Recovery
National Council for Behavioral Health
Mental Health Center of Denver Reaching Recovery
National Council for Behavioral Health