System Outcomes
250 Quality Measures for Individuals with Behavioral Health Disorders
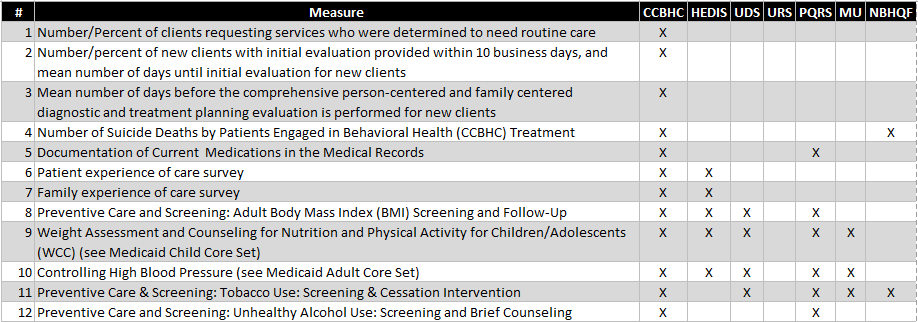
In the last several years seven National Quality Reporting Programs have focused effort to identify 250 quality measures that are relevant to individuals with behavioral health disorders. These include:
In the last several years seven National Quality Reporting Programs have focused effort to identify 250 quality measures that are relevant to individuals with behavioral health disorders. These include:
- The Certified Community Behavioral Health Clinic (CCBHC) program that was part of the 2014 Excellence in Mental Health Act (32 measures);
- The National Committee for Quality Assurance’s (NCQA) Healthcare Effectiveness Data and Information Set (HEDIS) (29 measures);
- The Bureau of Primary Health Care’s Uniform Data System (UDS) for Federally Qualified Health Centers (FQHCs) and Rural Health Centers (RHCs) (26 measures);
- The Centers for Medicare & Medicaid Services’ (CMS) Physician Quality Reporting System (PQRS) (41 measures);
- The Medicare and Medicaid EHR Incentive Programs (Meaningful Use) (67 measures);
- SAMHSA’s Uniform Reporting System (URS) that collects behavioral health-related performance measures from States, including the National Outcome Measures (NOMS) (27 measures);
- SAMHSA’s National Behavioral Health Quality Framework (NBHQF) (113 measures).
The full list of measures can be downloaded here.
Implementing a Systems Outcomes Measurement Process
Where do the RBHAs and Providers start when it comes to identifying what measures to track? We have three suggestions.
1. Build on the Existing Framework: The State of Arizona has a Performance Measurement Framework that will continue to evolve and serve as the foundation for Systems Outcome Measurement. The 2014 measures can be downloaded here. In addition, AHCCCS has worked with the Medicaid Health Plans to identify a set of Value-Based Purchasing measures that would be used by all of the Health Plans.
2. Consider the CCBHC Measures: The new Certified Community Behavioral Health Clinic is likely to be the foundation for the transformation of the community behavioral health system in the United States. There is funding for CCHBC Planning Grants that will lead to the selections of eight states that will share $1 billion to pilot the CCBHC program for two years. More information can be found at http://www.samhsa.gov/grants/grant-announcements/sm-16-001.
States that are interested in leveraging this opportunity will need to implement the 17 CCBHC-level Measures and 15 State Required Reporting Measures, all of which should be integrated into the AHCCCS/DBHS Performance Measurement Framework.
Where do the RBHAs and Providers start when it comes to identifying what measures to track? We have three suggestions.
1. Build on the Existing Framework: The State of Arizona has a Performance Measurement Framework that will continue to evolve and serve as the foundation for Systems Outcome Measurement. The 2014 measures can be downloaded here. In addition, AHCCCS has worked with the Medicaid Health Plans to identify a set of Value-Based Purchasing measures that would be used by all of the Health Plans.
2. Consider the CCBHC Measures: The new Certified Community Behavioral Health Clinic is likely to be the foundation for the transformation of the community behavioral health system in the United States. There is funding for CCHBC Planning Grants that will lead to the selections of eight states that will share $1 billion to pilot the CCBHC program for two years. More information can be found at http://www.samhsa.gov/grants/grant-announcements/sm-16-001.
States that are interested in leveraging this opportunity will need to implement the 17 CCBHC-level Measures and 15 State Required Reporting Measures, all of which should be integrated into the AHCCCS/DBHS Performance Measurement Framework.
|
CCBHC Measures
|
State Required Reporting Measures
|
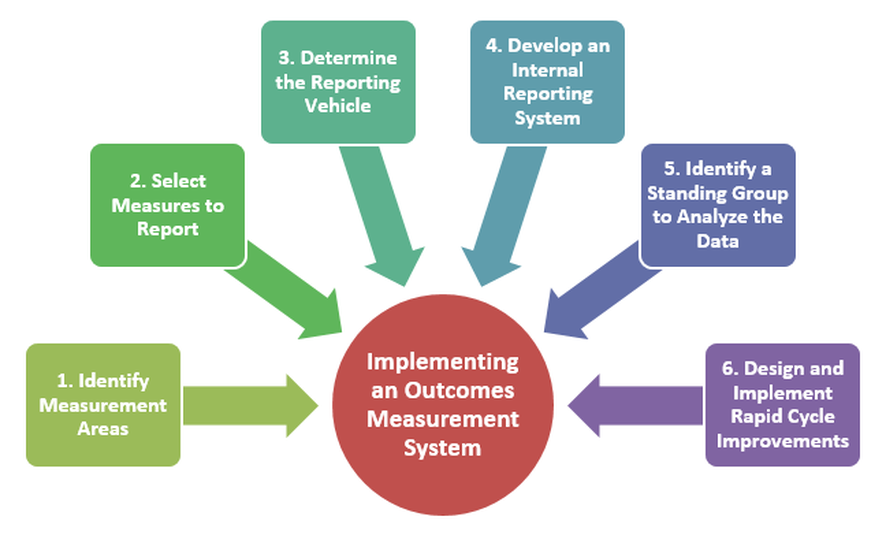
3. Develop a Well Organized Implementation Process: The following diagram illustrates a best-practice process for implementing a performance measurement system.