Sub-Capitation + P4P
While a simple concept, the terms Capitation and Sub-Capitation have morphed into a variety of meanings. For purposes of this Toolkit, we are going to use the following definitions.
Capitation Definition: An agreed upon payment from the Purchaser (Medicaid, Employer, Trade Union, etc.) to a Health Plan, paid in the form of a Per Member Per Month (PMPM) for each person who is enrolled with the Health Plan. In return for the PMPM, the Health Plan will assure timely access to a predefined set of health benefits and quality agreements that are provided by a Network of Providers that contract with the Health Plan as well as Out of Network Providers who bill outside a contractual relationship with the Health Plan.
Sub-Capitation Definition: An agreed upon payment from the Health Plan to a Provider Organization, including Accountable Care Organizations, paid in the form of a Per Member Per Month (PMPM) for each person who is assigned to the Provider Organization/ACO. In return for the PMPM, the Health Plan will assure timely access to a predefined set of health benefits and quality agreements, and the payment flows regardless of whether an individual uses services or not.
To restate, Purchasers pay Health Plans Capitation. Health Plans pay Provider Organizations/Groups Sub-Capitation. Capitation and Sub-Capitation are Population-Based Payments.
Sub-Capitation + P4P Definition: An agreed upon payment from the Health Plan to a Provider Organization, including Accountable Care Organizations, paid in the form of a Per Member Per Month (PMPM) for each person who is assigned to the Provider Organization/ACO. This model also includes a Pay for Performance bonus layer to incentivize better care, better health, and better cost. P4P is discussed in detail in the P4P section.
Why Be Picky About Words?
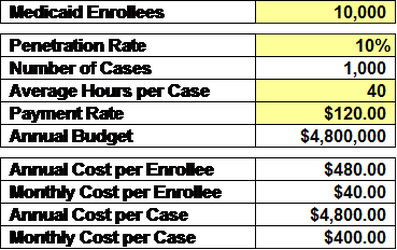
We know that only a fraction of Health Plan enrollees will require Behavioral Health services during the course of a year – generally 10% to 20%. Sometimes payments from Health Plans to Providers for those using Behavioral Health services are call Capitation or Sub-Capitation, which muddies the water. Let’s illustrate this muddiness.
Question 1: Based on the above figures is the Monthly Sub-Capitation Rate $40 or $400?
Answer 1a: If you follow the definitions listed above, it’s the Monthly Cost per Enrollee (PMPM), which is $40.00 (based on the Total Budget ($4,800,000) divided by the number of Enrollees (10,000) divided by 12 months).
Answer 1b: If you haven’t agreed upon a formal definition, it could be $40 or $400, which is confusing and not helpful.
Question 2: What do you call the Annual Cost per Case or Monthly Cost per Case?
Answer 2: The Annual Cost per Case or Monthly Cost per Case is called a Case Rate or Bundled Payment.
When You Should and Should NOT Use Sub-Capitation?
There’s an important logic thread from above that helps answer this question.
Sub-Capitation can only be used in a setting where the entire enrollment base can be assigned to one or more Provider Organizations/Groups. Below are examples of two situations where this is workable.
Sub-Capitation does NOT work well in the following situation:
Capitation Definition: An agreed upon payment from the Purchaser (Medicaid, Employer, Trade Union, etc.) to a Health Plan, paid in the form of a Per Member Per Month (PMPM) for each person who is enrolled with the Health Plan. In return for the PMPM, the Health Plan will assure timely access to a predefined set of health benefits and quality agreements that are provided by a Network of Providers that contract with the Health Plan as well as Out of Network Providers who bill outside a contractual relationship with the Health Plan.
Sub-Capitation Definition: An agreed upon payment from the Health Plan to a Provider Organization, including Accountable Care Organizations, paid in the form of a Per Member Per Month (PMPM) for each person who is assigned to the Provider Organization/ACO. In return for the PMPM, the Health Plan will assure timely access to a predefined set of health benefits and quality agreements, and the payment flows regardless of whether an individual uses services or not.
To restate, Purchasers pay Health Plans Capitation. Health Plans pay Provider Organizations/Groups Sub-Capitation. Capitation and Sub-Capitation are Population-Based Payments.
Sub-Capitation + P4P Definition: An agreed upon payment from the Health Plan to a Provider Organization, including Accountable Care Organizations, paid in the form of a Per Member Per Month (PMPM) for each person who is assigned to the Provider Organization/ACO. This model also includes a Pay for Performance bonus layer to incentivize better care, better health, and better cost. P4P is discussed in detail in the P4P section.
Why Be Picky About Words?
We know that only a fraction of Health Plan enrollees will require Behavioral Health services during the course of a year – generally 10% to 20%. Sometimes payments from Health Plans to Providers for those using Behavioral Health services are call Capitation or Sub-Capitation, which muddies the water. Let’s illustrate this muddiness.
Question 1: Based on the above figures is the Monthly Sub-Capitation Rate $40 or $400?
Answer 1a: If you follow the definitions listed above, it’s the Monthly Cost per Enrollee (PMPM), which is $40.00 (based on the Total Budget ($4,800,000) divided by the number of Enrollees (10,000) divided by 12 months).
Answer 1b: If you haven’t agreed upon a formal definition, it could be $40 or $400, which is confusing and not helpful.
Question 2: What do you call the Annual Cost per Case or Monthly Cost per Case?
Answer 2: The Annual Cost per Case or Monthly Cost per Case is called a Case Rate or Bundled Payment.
When You Should and Should NOT Use Sub-Capitation?
There’s an important logic thread from above that helps answer this question.
Sub-Capitation can only be used in a setting where the entire enrollment base can be assigned to one or more Provider Organizations/Groups. Below are examples of two situations where this is workable.
- Health Home-Based PMPM: Every enrollee is assigned to a Primary Care Provider working in a Health Home; the parents of the Health Homes (an ACO, Health System, Independent Practice Association, etc.) become the accountable organization and receive a PMPM Sub-Capitation payment. This can be in the form of a Primary Care Sub-Capitation Payment (for primary care services) or a Global Sub-Capitation Payment (for all services).
- Geographic Based PMPM: A defined geographic region (e.g. county) has only a small number of Behavioral Health Provider Organizations. Each person in the enrollment base can be assigned to one provider based on a predetermined algorithm. Each Behavioral Health Provider Organization is paid a Behavioral Health Sub-Capitation payment in the form of a PMPM for those in service and those who may never need service. Any individual who is in need of behavioral health services for the first time can go where they want for care and if it’s at a different organization, their assignment and PMPM will shift.
Sub-Capitation does NOT work well in the following situation:
- Large Population/Many Behavioral Health Providers: In a geographic area with a large population and a large number of providers. Using the above definition of Sub-Capitation, it’s practically unworkable to assign the entire enrollment base to one of many Behavioral Health Provider Organizations on a PMPM basis when only a portion of those individuals will actually present for care in a given year.
