Service Delivery Redesign

This section of the Toolkit contains five topics.
- Behavioral Health and Population Health
- A New Standard of Care for Persons with Behavioral Health Disorders
- Behavioral Health inside Health Homes
- Behavioral Health Centers of Excellence
- Community-Based Care
Behavioral Health and Population Health
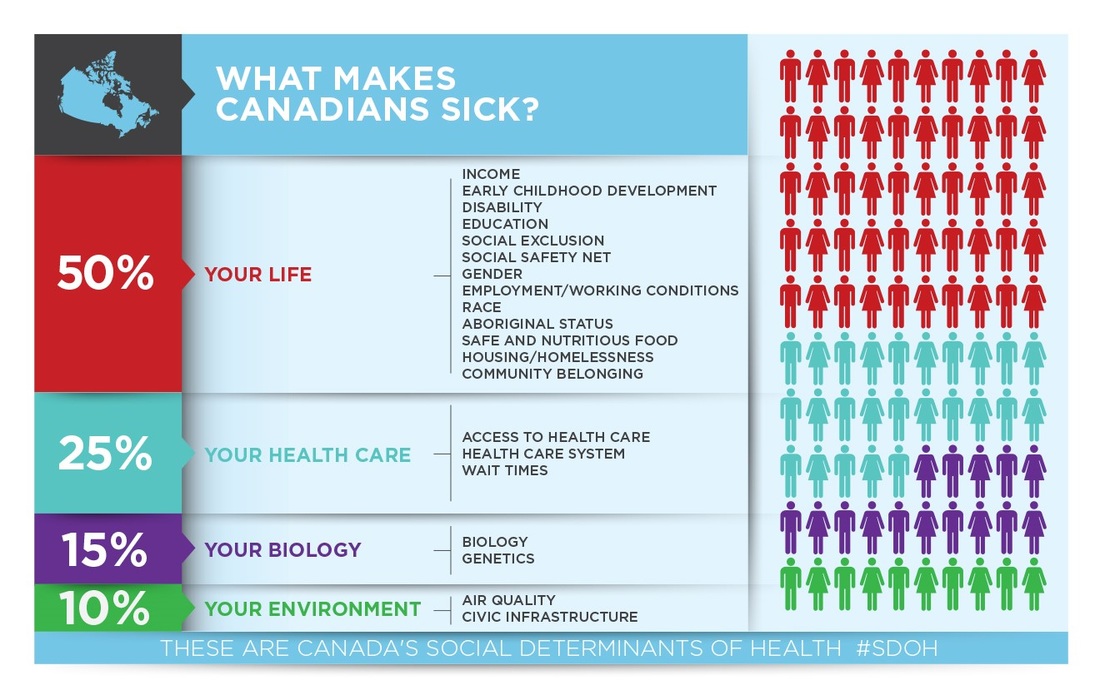
There is a great deal of evidence that health care makes up a small fraction of what determines health. The 25% slice in the infographic below includes medical care as well as behavioral healthcare.
As the U.S. moves from what is now a ‘sick care’ system to a true ‘health system’, medical and behavioral health provider organizations are being expected to address the whole health and well-being of the target populations they serve, including those currently in service as well as those in need but not yet in care. This creates a new ‘job description’ for community behavioral healthcare organizations that includes focusing on the following issues for the target populations they serve, which are drawn from the U.S. Department of Health and Human Services Healthy People 2020 initiative.

Neighborhood and Build Environment
- Access to healthy foods
- Access to quality housing
- Protection from crime and violence
- Access to a healthy environment (e.g. air quality, clean water supply)
“But this isn’t my job!”
Although there are limits to what behavioral health organizations and providers can accomplish, the emerging new normal is, the expectation of ‘relieving symptoms’ is being replaced with the expectation to support healthy individual, healthy families, and healthy communities.
Although there are limits to what behavioral health organizations and providers can accomplish, the emerging new normal is, the expectation of ‘relieving symptoms’ is being replaced with the expectation to support healthy individual, healthy families, and healthy communities.
A New Standard of Care for Persons with Behavioral Health Disorders
There is an emerging standard of care for the screening, assessment and treatment of persons with behavioral health disorders that is increasing the number of people with behavioral health disorders being engaged in care that works. This new standard looks very much like the current standards of care for diabetes and hypertension treatment and is forcing us to rethink everything we’ve thought about the use rates of mental health and substance use disorder treatment.
Primary care providers are now expected to screen youth, adolescents, adults and elders for mental health (MH) and substance use (SU) disorders. If there is evidence of a MH/SU problem, the primary care provider will do a warm hand-off to a behavioral health professional working in the clinic. If a full assessment determines that there is a condition that will benefit from treatment, the behavioral health professional will work to engage the individual and develop an evidence-based care plan and self-care plan that leads to outcomes-based treatment.
Behavioral health providers are now expected to screen youth, adolescents, adults and elders for physical health conditions. If there is evidence of a health problem, a care manager at the behavioral health clinic becomes part of the care team. Their job is to further assess the problem, engage the individual in active treatment with their primary care provider (PCP), and serve as an extender for the PCP, supporting the development of an integrated care plan and self-care plan, monitoring the condition(s), and ensuring that progress is being made toward full management of their health and behavioral health conditions.
This two-part standard of care is leading to the evolution of three types of integrated care settings.
Primary care providers are now expected to screen youth, adolescents, adults and elders for mental health (MH) and substance use (SU) disorders. If there is evidence of a MH/SU problem, the primary care provider will do a warm hand-off to a behavioral health professional working in the clinic. If a full assessment determines that there is a condition that will benefit from treatment, the behavioral health professional will work to engage the individual and develop an evidence-based care plan and self-care plan that leads to outcomes-based treatment.
Behavioral health providers are now expected to screen youth, adolescents, adults and elders for physical health conditions. If there is evidence of a health problem, a care manager at the behavioral health clinic becomes part of the care team. Their job is to further assess the problem, engage the individual in active treatment with their primary care provider (PCP), and serve as an extender for the PCP, supporting the development of an integrated care plan and self-care plan, monitoring the condition(s), and ensuring that progress is being made toward full management of their health and behavioral health conditions.
This two-part standard of care is leading to the evolution of three types of integrated care settings.
Behavioral Health inside Health Homes
Behavioral Health providers are becoming deeply embedded in primary care teams providing prevention and early intervention services, addressing health behaviors as well as treating behavioral health disorders. These staff are also supporting the whole health needs of their clients by helping ensure that individuals with behavioral health disorders have integrated, whole health care plans.
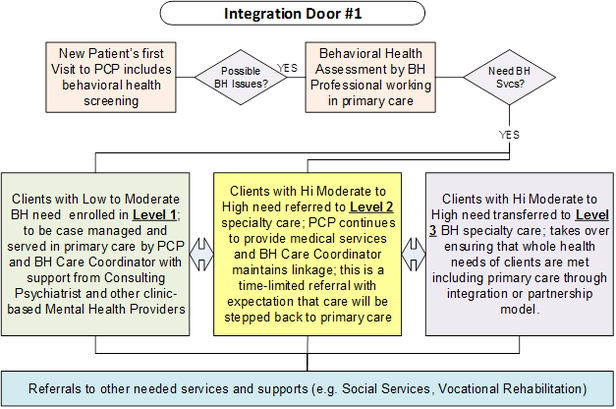
The diagram (Integration Door #1) illustrates an emerging workflow that describes how all patients are receiving a behavioral health screening from their Primary Care Provider (PCP) and if there are possible Behavioral Health (BH) issues, a warm handoff is made to a Behavioral Health Professional who works in the clinic.
Individuals with behavioral health disorders can have their behavioral healthcare provided in the primary care clinic (Level 1); at a behavioral health specialty clinic while continuing to receive their primary care at the primary care clinic (Level 2); or have their entire care transferred to a specialty behavioral health clinic with embedded primary care (Level 3). This affords clients three options for receiving integrated care.
This approach aligns with the evolution of Patient Centered Medical Homes, which is increasingly acknowledging the importance of behavioral health to whole health.
A sampling of integration references from leading organizations includes:
The diagram (Integration Door #1) illustrates an emerging workflow that describes how all patients are receiving a behavioral health screening from their Primary Care Provider (PCP) and if there are possible Behavioral Health (BH) issues, a warm handoff is made to a Behavioral Health Professional who works in the clinic.
Individuals with behavioral health disorders can have their behavioral healthcare provided in the primary care clinic (Level 1); at a behavioral health specialty clinic while continuing to receive their primary care at the primary care clinic (Level 2); or have their entire care transferred to a specialty behavioral health clinic with embedded primary care (Level 3). This affords clients three options for receiving integrated care.
This approach aligns with the evolution of Patient Centered Medical Homes, which is increasingly acknowledging the importance of behavioral health to whole health.
A sampling of integration references from leading organizations includes:
Behavioral Health Centers of Excellence
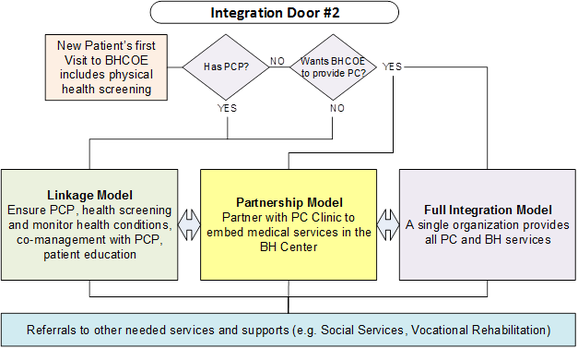
Behavioral Health Centers of Excellence (BHCOEs) are high performing specialty mental health, substance use disorder, and co-occurring disorder treatment organizations that partner with health homes, providing high value, whole health-oriented, specialty care to individuals with complex behavioral health conditions. The following diagram (Integration Door #2) illustrates how people’s whole health needs can be met beginning with their first contact with a BHCOE.
Every new patient’s first visit includes a physical health screening and assistance with obtaining a primary care provider if the patient doesn’t already have one. Primary care can be provided at a primary care that has a linkage relationship with the BHCOE (Linkage Model); or onsite at the BHCOE. Onsite primary care is provided by a separate primary care clinic that has a satellite office at the BHCOE (Partnership Model); or by the BHCOE itself, which has employed primary care staff (Full Integration Model).
The Behavioral Health Center of Excellence effort began with a two-year crowdsourcing project undertaken by the National Council for Behavioral Health, starting in 2013. This effort led to the definition of a BHCOE and the identification of five core elements:
For more information, visit: http://www.thenationalcouncil.org/wp-content/uploads/2013/12/BHCOE-draft-FINAL-12-18-13.pdf
The BHCOE design work is reflected in the new Certified Community Behavioral Health Clinic (CCBHC) legislation that was passed in March 2014 to establish a parallel system to Federally Qualified Health Centers.
Additional resources on CCBHCs include:
Every new patient’s first visit includes a physical health screening and assistance with obtaining a primary care provider if the patient doesn’t already have one. Primary care can be provided at a primary care that has a linkage relationship with the BHCOE (Linkage Model); or onsite at the BHCOE. Onsite primary care is provided by a separate primary care clinic that has a satellite office at the BHCOE (Partnership Model); or by the BHCOE itself, which has employed primary care staff (Full Integration Model).
The Behavioral Health Center of Excellence effort began with a two-year crowdsourcing project undertaken by the National Council for Behavioral Health, starting in 2013. This effort led to the definition of a BHCOE and the identification of five core elements:
- World class customer service built on a culture of staff and client engagement and wellness
- Excellent outcomes
- Easy access
- Comprehensive care
- Excellent value
For more information, visit: http://www.thenationalcouncil.org/wp-content/uploads/2013/12/BHCOE-draft-FINAL-12-18-13.pdf
The BHCOE design work is reflected in the new Certified Community Behavioral Health Clinic (CCBHC) legislation that was passed in March 2014 to establish a parallel system to Federally Qualified Health Centers.
Additional resources on CCBHCs include:
Community-Based Care
 (Image courtesy of graur razvan ionut at FreeDigitalPhotos.net)
(Image courtesy of graur razvan ionut at FreeDigitalPhotos.net)
The healthcare delivery system that evolved over the last forty years was organized around a provider-centric model of care. Under this approach, all routine health and behavioral healthcare has been organized during 9 to 5 business hours at a clinic site, often scheduled days and weeks in advance at an appointed time. This model, particularly for individuals with serious and severe behavioral health disorders, is often not responsive to patient needs and results in high no-show rates.
An emerging model is moving the locus of care to where people live, work, and spend their time. This includes onsite workplace clinics, home visits, and clinicians deployed to schools, nursing homes, supportive housing, youth centers, etc. Care is provided by community-based individuals and teams whose home based in the Health Home or Behavioral Health Center of Excellence.
An emerging model is moving the locus of care to where people live, work, and spend their time. This includes onsite workplace clinics, home visits, and clinicians deployed to schools, nursing homes, supportive housing, youth centers, etc. Care is provided by community-based individuals and teams whose home based in the Health Home or Behavioral Health Center of Excellence.