Value-Based Purchasing Basics
Value-Based Purchasing Definition
Value-Based Purchasing is also known as moving from “paying for volume” to “paying for value”.
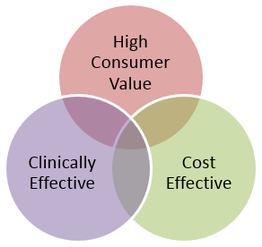
In a Value-Based Purchasing (VBP) environment, payors hold providers accountable for both the Cost and Quality of Care. This is done through the use of strategies to reward providers for reducing inappropriate care and providing high value care that is patient centered, clinically effective, and cost effective care.
“This strategy can be contrasted with more limited efforts to negotiate price discounts, which reduce costs but do little to ensure that quality of care is improved." “Value-based purchasing brings together information on the quality of health care, including patient outcomes and health status, with data on the dollar outlays going towards health.” (Meyer J, Rybowski L, Eichler R. Theory and Reality of Value-Based Purchasing: Lessons from the Pioneers. Rockville, MD: Agency for
Health Care Policy and Research; 1997. AHCPR Publication No. 98-0004.)
Let’s unpack the three components of high value care.
Patient Centered: The care is easily accessible and provided by staff that communicate well, demonstrate knowledge and technical proficiency, and take enough time to address the needs of the client; (http://forces4quality.org/node/6805)
Clinically Effective: The care is effective in achieving individual outcomes that matter to clients and system-wide outcomes that matter to payors and the community;
Cost Effective: The care is more cost-effective than alternatives that may have been selected because of the treatment selected and/or because waste (excess costs) has been removed from the work processes.
Reduction in inappropriate care and widespread use of high value care is synonymous with achieving the triple aim of better care, better health and better cost.
Value-Based Purchasing is also known as moving from “paying for volume” to “paying for value”.
In a Value-Based Purchasing (VBP) environment, payors hold providers accountable for both the Cost and Quality of Care. This is done through the use of strategies to reward providers for reducing inappropriate care and providing high value care that is patient centered, clinically effective, and cost effective care.
“This strategy can be contrasted with more limited efforts to negotiate price discounts, which reduce costs but do little to ensure that quality of care is improved." “Value-based purchasing brings together information on the quality of health care, including patient outcomes and health status, with data on the dollar outlays going towards health.” (Meyer J, Rybowski L, Eichler R. Theory and Reality of Value-Based Purchasing: Lessons from the Pioneers. Rockville, MD: Agency for
Health Care Policy and Research; 1997. AHCPR Publication No. 98-0004.)
Let’s unpack the three components of high value care.
Patient Centered: The care is easily accessible and provided by staff that communicate well, demonstrate knowledge and technical proficiency, and take enough time to address the needs of the client; (http://forces4quality.org/node/6805)
Clinically Effective: The care is effective in achieving individual outcomes that matter to clients and system-wide outcomes that matter to payors and the community;
Cost Effective: The care is more cost-effective than alternatives that may have been selected because of the treatment selected and/or because waste (excess costs) has been removed from the work processes.
Reduction in inappropriate care and widespread use of high value care is synonymous with achieving the triple aim of better care, better health and better cost.
Value-Based Purchasing Elements

A successful Value-Based Purchasing (VBP) environment will contain the following elements.
Element One – Standardized Performance Measurement: In order to measure value, stakeholders must agree upon and implement a set of performance measures that support measurement of the three elements of high value care: patient centered, clinically effective, and cost effective. This should also include transparency and public reporting of the results. This topic is further explored in the Performance Measurement Section of this Toolkit.
Element One – Standardized Performance Measurement: In order to measure value, stakeholders must agree upon and implement a set of performance measures that support measurement of the three elements of high value care: patient centered, clinically effective, and cost effective. This should also include transparency and public reporting of the results. This topic is further explored in the Performance Measurement Section of this Toolkit.
 (Image courtesy of atibodyphoto at FreeDigitalPhotos.net)
(Image courtesy of atibodyphoto at FreeDigitalPhotos.net)
Element Two – Accountable Payment Models: Moving to value-based purchasing also requires the use of Accountable Payment Models where the financial reward is embedded in the payment model. We believe that four payment models are appropriate for Behavioral Health: Capacity-Based, Fee for Service, Case Rate/Bundled Payment, and Sub-Capitation. These are described in detail throughout this Section.
Element Three – Pay for Performance: Moving to value-based purchasing requires the use of a payment approach where high performing providers are directly rewarded for the efforts to successfully provide patient centered, clinically effective, and cost effective care. This is examined in detail in this Section. below.
Element Three – Pay for Performance: Moving to value-based purchasing requires the use of a payment approach where high performing providers are directly rewarded for the efforts to successfully provide patient centered, clinically effective, and cost effective care. This is examined in detail in this Section. below.

Element Four – Balancing the Funding Portfolio: Allocating dollars to achieve the proper balance of spending across the service array is often needed to correct existing imbalances that prevent reaching better care and better health. Examples include ensuring adequate spending on primary prevention to reduce the need for treatment of preventable illness and higher spending on health homes to reduce the use of crisis and emergency room use as well as medical and psychiatric inpatient admissions. This topic is discussed in further detail in the System Modeling Section of this Toolkit.
Transitioning to Value-Based Purchasing
Moving to Value-Based Purchasing is a marathon, not a sprint, due to the decades of infrastructure and culture that have been laid down to support paying for volume, not value. Value-Based Purchasing succeeds best when the Payors and Providers work together to identify a multi-phase transition plan that increases provider accountability for quality and cost over time. There are no quick fixes for achieving the triple aim.
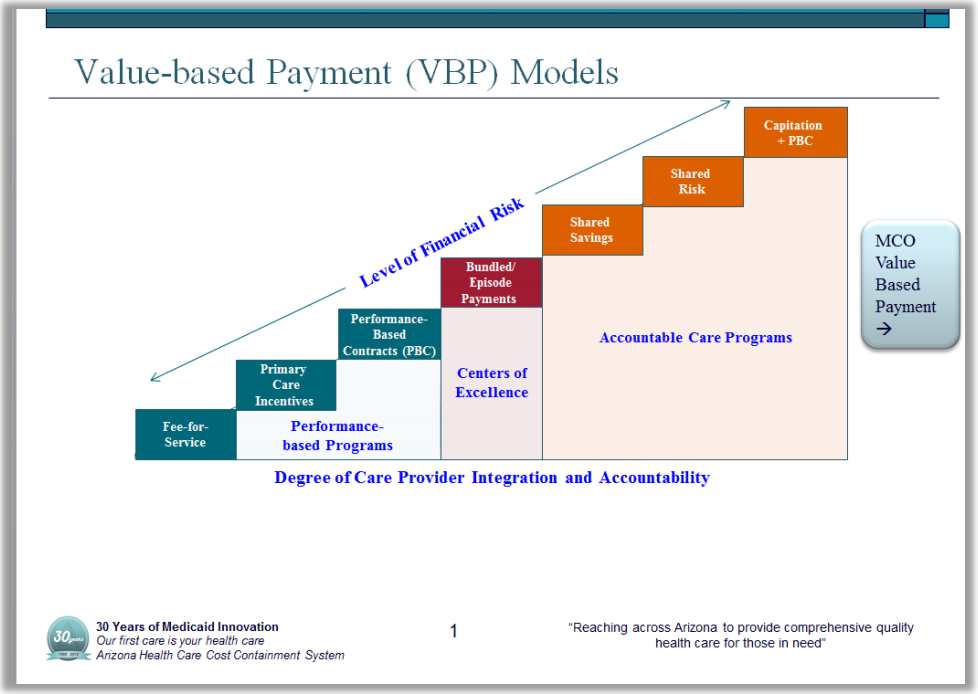
AHCCCS has been working on Healthcare Value-Based Purchasing (VBP) for a number of year and has developed the following diagram to illustrate the healthcare VBP journey.
AHCCCS has been working on Healthcare Value-Based Purchasing (VBP) for a number of year and has developed the following diagram to illustrate the healthcare VBP journey.
This approach shows the Accountable Payment Models on the same continuum as the Pay for Performance strategies, illustrating how increasing financial risk corresponds to increasing provider integration and accountability – a very important construct.
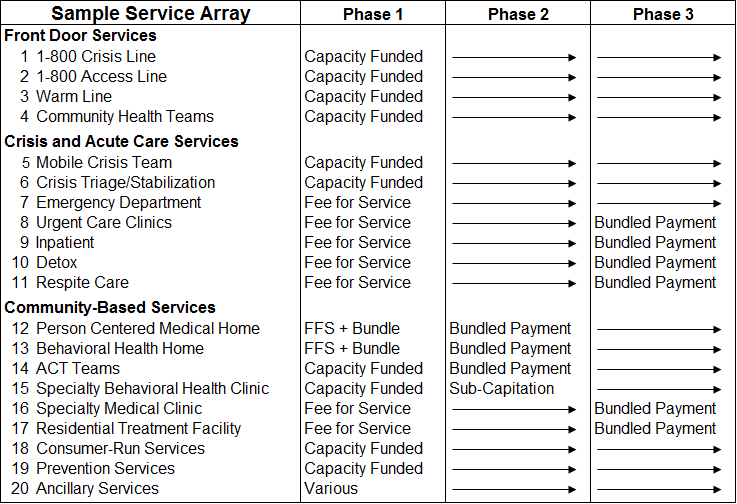
The following Sample Behavioral Health Payment Reform Transition Plan provides an example of how this transition could occur in the RBHA system. Each RBHA will need to work with their Provider Network to design a plan based on the unique facts and circumstances of their local ecosystem, keeping in mind the key concepts described in this Toolkit.
The following Sample Behavioral Health Payment Reform Transition Plan provides an example of how this transition could occur in the RBHA system. Each RBHA will need to work with their Provider Network to design a plan based on the unique facts and circumstances of their local ecosystem, keeping in mind the key concepts described in this Toolkit.
|
Phase 1 – Payment Reform Preparation
|
Phase 2 – Begin Pay for Performance
|
Phase 3 – Full Value-Based Purchasing
|
One Size Does NOT Fit All
A system of care for individuals with behavioral health disorders is comprised of a broad array of services, some of which are unique to the population. It is essential to examine each category of service and identify which Pay for Performance Model and which Accountable Payment Model fits best for that service category. One size does NOT fit all.
The second essential concept builds on the Transitioning to Value-Based Purchasing Section – It is important to PHASE IN Performance Models and which Accountable Payment Models based on Providers’ abilities to successfully operate under the models and RBHAs’ abilities to administer the models.
The following diagram provides an example of a Service Array and three potential phases of Accountable Payment Models. Note that the four types of Payment Models are defined in the Accountable Payment Models section below.
Important Note: Each RBHA will need to develop their own version of this diagram and a template can be downloaded at: [www.weblink-here.com]
The second essential concept builds on the Transitioning to Value-Based Purchasing Section – It is important to PHASE IN Performance Models and which Accountable Payment Models based on Providers’ abilities to successfully operate under the models and RBHAs’ abilities to administer the models.
The following diagram provides an example of a Service Array and three potential phases of Accountable Payment Models. Note that the four types of Payment Models are defined in the Accountable Payment Models section below.
Important Note: Each RBHA will need to develop their own version of this diagram and a template can be downloaded at: [www.weblink-here.com]
Value-Based Purchasing Management Structures
In order to succeed under Behavioral Health Value-Based Purchasing, a solid authorization and utilization management foundation must be built.
Last Generation Authorization and Utilization Management Criteria: The older generation of managed care was structured so that the payor hired a large number of expensive employees to do three things:
This was a very labor intensive and expensive proposition for payors and providers and generated a great deal of blowback from providers and patients.
Modern Authorization and Utilization Management Criteria: The current generation of managed care is based on modern quality improvement principles that support a managed structure that is shared by the payor and providers. In behavioral health this approach contains the following components. This design is then used to support the four types of Accountable Payment Models.
Last Generation Authorization and Utilization Management Criteria: The older generation of managed care was structured so that the payor hired a large number of expensive employees to do three things:
- Write long Pre-Authorization and Utilization Management Guidelines documents that could be used to justify not paying for care;
- Pre-Authorize large numbers of services before those services could be provided;
- Do extensive Concurrent Review in order to look for services that didn’t meet the rules and could be denied.
This was a very labor intensive and expensive proposition for payors and providers and generated a great deal of blowback from providers and patients.
Modern Authorization and Utilization Management Criteria: The current generation of managed care is based on modern quality improvement principles that support a managed structure that is shared by the payor and providers. In behavioral health this approach contains the following components. This design is then used to support the four types of Accountable Payment Models.
|
Level of Care System: The payors and providers create a level of care system that describes different levels of care with enough specificity that common agreement can be reached. Two systems that have been in place for many years are the ASAM Criteria, which are a comprehensive set of guidelines for placement, continued stay, and transfer/discharge of patients with addiction and co-occurring conditions; and the LOCUS (Level of Care Utilization System) for behavioral health. A number of states and regional system have implemented these and other similar systems in order to create a self-management foundation. Generally these systems provide definition for at least inpatient, residential, and multiple levels of outpatient care.
|
Utilization Management Guidelines: Once the Levels of Care are identified, Utilization Management Guidelines are developed for each level of care, including:
|
Self-Management Rules: The payor and providers will agree on which levels can be self-authorized (most levels), which levels require pre-authorization (only the highest), and how concurrent review will be managed (less review for providers who follow the rules).
|
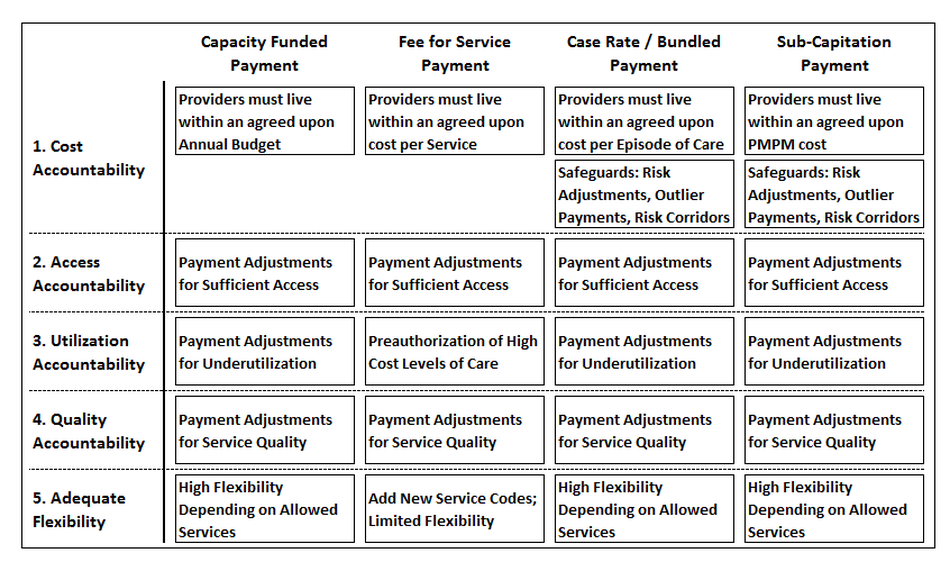
Value-Based Purchasing Accountability Matrix
The four Accountable Payment Models combined with Pay for Performance (P4P) layers are designed to work together to increase provider accountability in ways that are described in the following diagram.
The diagram, which lists the four Payment Models in the columns, examines each from five perspectives:
- Cost Accountability: The Payment Model determines whether Financial Risk related to Cost, Individual Utilization, Case Mix and Penetration are transferred from the Payor to the Provider. It is also important to consider Provider/Payor Safeguards when Case Rates/Bundled Payments or Subcapitation is paid. The narrative in row 1 summarizes these hydraulics. The Risk/Reward Equation material immediately below and the Extra Credit Section of this Toolkit go into greater detail on this topic.
- Access Accountability: All four payment models ideally should contain performance standards related to Access that are connected to the Pay for Performance (P4P) design. This is explored further in the Pay for Performance Section of this Toolkit.
- Utilization Accountability: Three of the four payment models create a Provider incentive for underutilization. To address this, the Value-Based Purchasing Plan should contain performance standards related to Utilization that are part of the Pay for Performance (P4P) design. This is explored further in the Pay for Performance Section of this Toolkit. With the Fee for Service Payment Model, overutilization is a concern, and Preauthorization for High Cost Levels of Care should be considered.
- Quality Accountability: All four payment models ideally should contain performance standards related to Quality that are connected to the Pay for Performance (P4P) design. This is explored further in the Pay for Performance Section of this Toolkit.
- Adequate Flexibility: Value-Based Purchasing only works if the Payment Model has sufficient flexibility to ensure the right care in the right setting by the right person. This is generally a design element of three of the payment models – if the Purchaser doesn’t overregulate the system. This is discussed in the Infrastructure Section of this Toolkit. This is not a part of Fee for Service and extra effort must be made to add greater flexibility to that payment model.