Why Behavioral
Health Payment Reform?
Why do we say that we cannot fix the healthcare quality and cost problems in the U.S. without better addressing the health and behavioral health needs of Americans with behavioral health disorders?
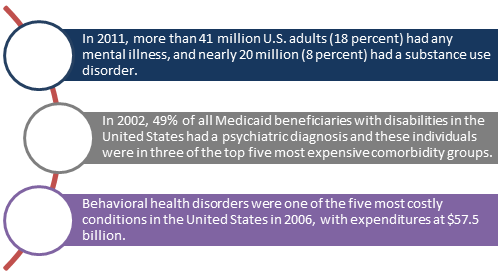
The answer is simple. This population, which is large in number, has high healthcare costs followed by early mortality. Half of the 5/50 population – the 5% of Americans that use 50% of the resources – is made up of individuals with behavioral health disorders.
Let’s take a moment to explore a few more important statistics.
The answer is simple. This population, which is large in number, has high healthcare costs followed by early mortality. Half of the 5/50 population – the 5% of Americans that use 50% of the resources – is made up of individuals with behavioral health disorders.
Let’s take a moment to explore a few more important statistics.
In 2006, the National Association of State Mental Health Program Directors published their landmark report, Morbidity and Mortality in People with Serious Mental Illness.
In that report we learned
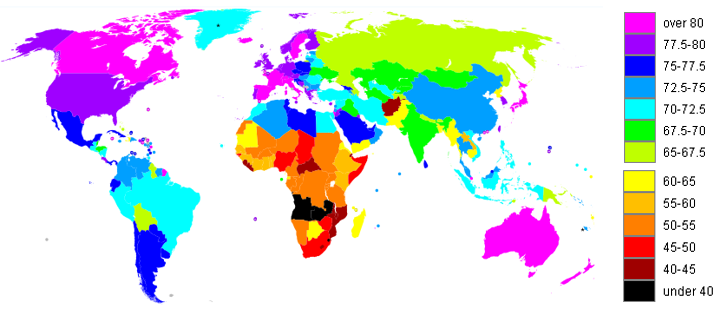
In the United States, the 53 year lifespan for people with serious mental illness is comparable to the residents of many countries in Sub-Saharan Africa.
Find the full report here.
In that report we learned
- Persons with serious mental illness are now dying 25 years earlier than the general population
- Increased mortality and morbidity are largely due to preventable health conditions – cardiovascular disease, diabetes, respiratory disease, infectious disease
In the United States, the 53 year lifespan for people with serious mental illness is comparable to the residents of many countries in Sub-Saharan Africa.
Find the full report here.
|
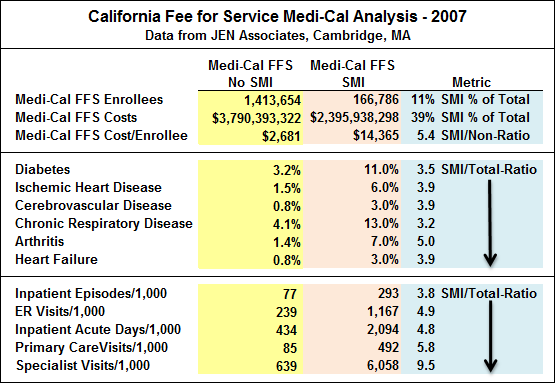
A study by JEN Associates for the State of California determined that individuals with serious mental illness (SMI) in California’s fee for service Medicaid system (Medi-Cal) had average healthcare costs that were 5.4 times higher than those without SMI. This was due to higher rates of chronic health conditions requiring higher use of inpatient, emergency (ER) and specialty medical care.
|
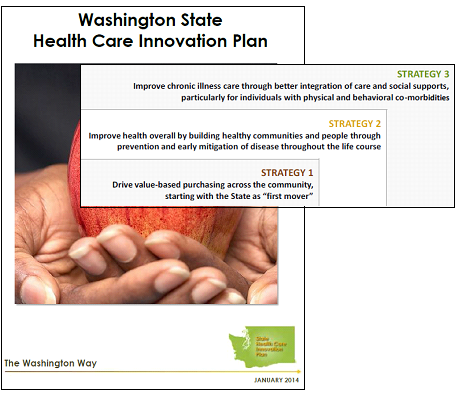
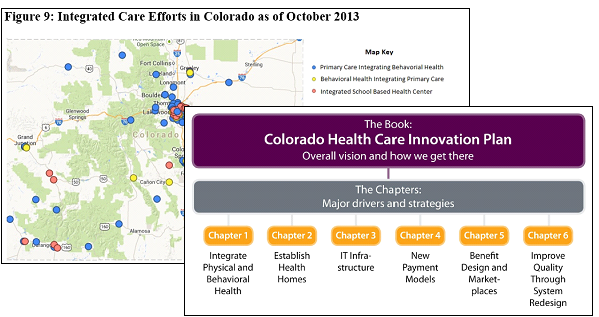
The federal government, states, counties, health plans and
business leaders are translating this information into action. Below are
examples from Washington State and Colorado that illustrate the importance of
behavioral health to the healthcare reform efforts in this country.