Pay for Performance At-a-Glance
The following infographic provides an at-a-glance view of how to implement a P4P program. (pdf available here.)
Pay for Performance
Pay for Performance can occur in two ways, discussed below:
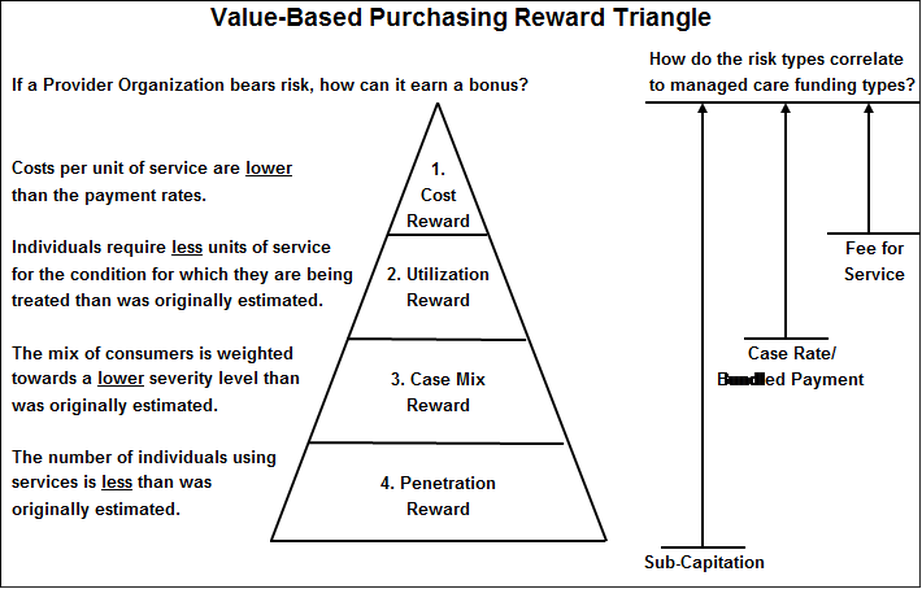
P4P Embedded in the Payment Model: Accountable Payment Models that push risk/reward down to the Provider through Case Rates or Sub-Capitation allows for an efficiency performance bonus as illustrated in the following diagram.
This is covered in more detail in other parts of the Payment Reform Section of the Toolkit.
- P4P Embedded in the Payment Model
- The P4P Layer
P4P Embedded in the Payment Model: Accountable Payment Models that push risk/reward down to the Provider through Case Rates or Sub-Capitation allows for an efficiency performance bonus as illustrated in the following diagram.
This is covered in more detail in other parts of the Payment Reform Section of the Toolkit.
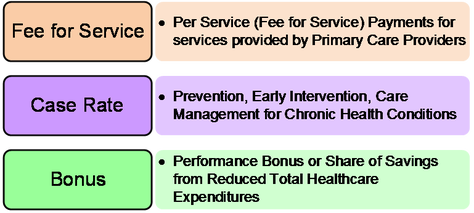
The P4P Layer: The second method is to add a performance layer on top of any of the payment model. This is illustrated by the following diagram, which is a common approach to funding Health Homes.
The clinic will continue to be paid Fee for Service for services that lend themselves to CPT and HCPC codes. A second payment in the form of a Case Rate is also paid to the clinic to cover Health Home services whose costs cannot be covered by CPT and HCPC codes such as prevention, early intervention, and care management for chronic health conditions. Added to those two payments is a Bonus Layer that can take two forms:
The clinic will continue to be paid Fee for Service for services that lend themselves to CPT and HCPC codes. A second payment in the form of a Case Rate is also paid to the clinic to cover Health Home services whose costs cannot be covered by CPT and HCPC codes such as prevention, early intervention, and care management for chronic health conditions. Added to those two payments is a Bonus Layer that can take two forms:
- Performance Bonus: A Performance Bonus that is made if the clinic meets or exceeds the agreed upon performance standards;
- Shared Savings Bonus: A Shared Savings Bonus that is a portion of the monies saved generally through reduction in emergency room, acute care hospital, diagnostic imaging, and/or medical specialty care.
The Performance Bonus
This part of the P4P section digs into the key steps listed on the infographic above.
This part of the P4P section digs into the key steps listed on the infographic above.
Step 1: Identify what's important.
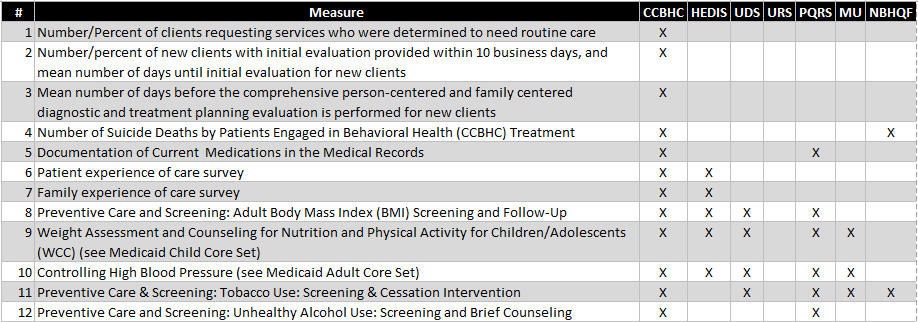
The Performance Measurement Section of this Toolkit goes into depth about the performance measures that have been identified as relevant to individuals with behavioral health disorders. This list is the starting point for developing the performance measures that are most important for the population being served.
The Performance Measurement Section of this Toolkit goes into depth about the performance measures that have been identified as relevant to individuals with behavioral health disorders. This list is the starting point for developing the performance measures that are most important for the population being served.
The full list of measures can be downloaded here.
Step 2: Select the vital few.
Adding too many Performance Measures to a Service Area generally fails because the cost and time needed to manage this type of design can cripple the ability of the clinicians to provide quality care. A short list of a “Vital Few” is always better, especially in the beginning of a P4P program.
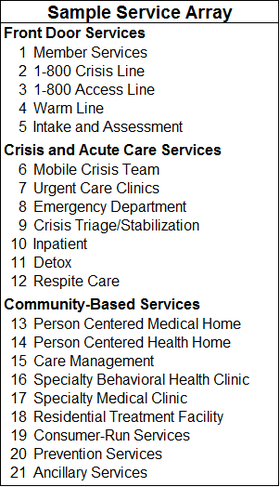
As illustrated by the table to the right, a Behavioral Health System of Care contains several service areas that addresses the totality of what individuals with behavioral health disorders need to address their behavioral health and healthcare needs.
We recommend a P4P program where all service areas have a Pay for Performance Bonus component. It is also critical to ensure that each service area is only held accountable for the performance measures relevant to the work they do. Thus the importance of mapping the relevant performance measures to each service population.
For most, if not all of the service areas, at least one Patient Experience, Access, and Clinical Quality Measure is critical, but the specific measures will vary by service area. For example, a Health Home should be taking responsibility for Diabetes-related measures; a Mobile Crisis team should not. An Emergency Department treating someone with a psychiatric emergency should be responsible for ensuring that a solid handoff occurs to a community behavioral health provider for ongoing care; a Prevention Services Program should not.
Step 3: Complete a Gap Analysis
Every system is at a different place in its journey to performance measurement. Providers and payors that have been collecting and reporting on data for years will be able to move into P4P much faster than systems that are new to this effort. Don’t underestimate how much infrastructure and new work processes are required to roll out a P4P system. Example requirements include:
Step 4: Revise and Phase your Design.
There are four potential phases for rolling out a P4P program, depending on the existing infrastructure:
Sometimes it’s possible to go straight to Phase 2 (Pay for Reporting) or even Phase 3 (Pay for Performance).
Step 5: Identify Baseline and Benchmark Metrics and Step 6: Develop your Payment Model
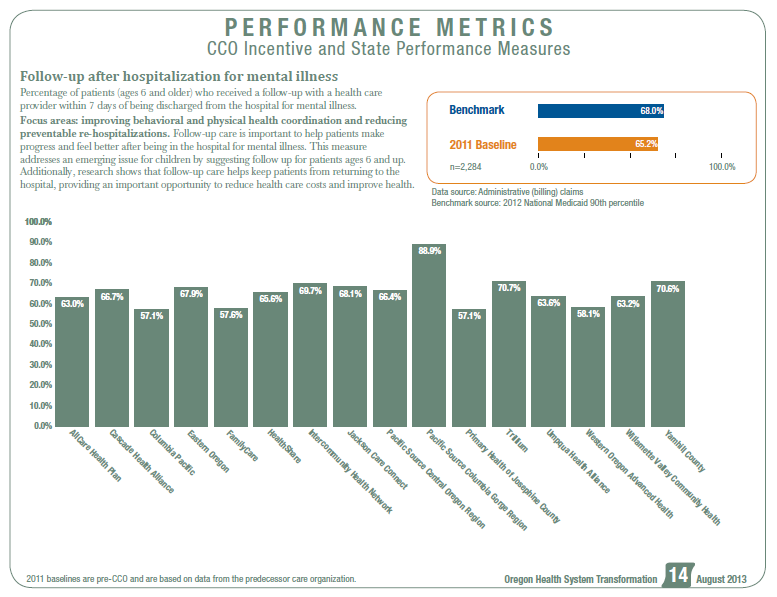
The following example from Oregon about Follow-up after hospitalization for mental illness illustrates Benchmarks and Baseline.
Benchmark: Oregon’s goal is that 68% or more of the individuals being discharged from the hospital for a psychiatric admission should receive a follow-up visit with a community based provider within 7 days.
2011 Baseline: In 2011 the 16 CCOs (Coordinated Care Organizations; Oregon’s version of a Medicaid Health Plans) had varying rates of patients who met the Benchmark, from a low of 57.1% in two of the CCOs to a high of 88.9%.
Providers earn their Bonus if they 1) Show Improvement or 2) Hit the Benchmark: Each CCO that either hit the 68% figure or did better than their baseline would earn their Incentive Bonus.
Step 2: Select the vital few.
Adding too many Performance Measures to a Service Area generally fails because the cost and time needed to manage this type of design can cripple the ability of the clinicians to provide quality care. A short list of a “Vital Few” is always better, especially in the beginning of a P4P program.
As illustrated by the table to the right, a Behavioral Health System of Care contains several service areas that addresses the totality of what individuals with behavioral health disorders need to address their behavioral health and healthcare needs.
We recommend a P4P program where all service areas have a Pay for Performance Bonus component. It is also critical to ensure that each service area is only held accountable for the performance measures relevant to the work they do. Thus the importance of mapping the relevant performance measures to each service population.
For most, if not all of the service areas, at least one Patient Experience, Access, and Clinical Quality Measure is critical, but the specific measures will vary by service area. For example, a Health Home should be taking responsibility for Diabetes-related measures; a Mobile Crisis team should not. An Emergency Department treating someone with a psychiatric emergency should be responsible for ensuring that a solid handoff occurs to a community behavioral health provider for ongoing care; a Prevention Services Program should not.
Step 3: Complete a Gap Analysis
Every system is at a different place in its journey to performance measurement. Providers and payors that have been collecting and reporting on data for years will be able to move into P4P much faster than systems that are new to this effort. Don’t underestimate how much infrastructure and new work processes are required to roll out a P4P system. Example requirements include:
- Provider Electronic Health Records systems that are able to collect data from clinical measurement tools such as the PHQ-9, ACORN, and DLA-20;
- The ability of providers to transmit measurement data and payors to receive those data in formats that allow for easy entry into a measurement database or data warehouse;
- The ability to house benchmark data for each measure and P4P success threshold levels;
- Measurement analysis and reporting systems to determine progress on each measure and whether the P4P bonus was met for each provider;
- Work processes at the provider level to collect the performance measurement data and enter into the billing or electronic health records systems;
- Audit processes at the provider level to determine whether data are being accurately recorded and input and where gaps in data collection are occurring;
- Adequate staffing and work processes at the payor level to manage the P4P system;
- P4P reconciliation processes at the provider level to determine the accuracy of the P4P results being reported by the provider;
Step 4: Revise and Phase your Design.
There are four potential phases for rolling out a P4P program, depending on the existing infrastructure:
- Pay for Participation: “We agree to participate in developing a ‘quality contract’ that describes the P4P design and measures.”
- Pay for Reporting: Additional payments to support the cost of moving to a P4P including implementation and use of health information technology.
- Pay for Performance: Pay for hitting process targets (68% of patients had follow-up visits within 7 days of hospital discharge).
- Pay for Success: Paying for whether the care is “working” (65% of patients have an A1c levels under 7; total health expenditure growth has declined from 6% per year to 4%).
Sometimes it’s possible to go straight to Phase 2 (Pay for Reporting) or even Phase 3 (Pay for Performance).
Step 5: Identify Baseline and Benchmark Metrics and Step 6: Develop your Payment Model
The following example from Oregon about Follow-up after hospitalization for mental illness illustrates Benchmarks and Baseline.
Benchmark: Oregon’s goal is that 68% or more of the individuals being discharged from the hospital for a psychiatric admission should receive a follow-up visit with a community based provider within 7 days.
2011 Baseline: In 2011 the 16 CCOs (Coordinated Care Organizations; Oregon’s version of a Medicaid Health Plans) had varying rates of patients who met the Benchmark, from a low of 57.1% in two of the CCOs to a high of 88.9%.
Providers earn their Bonus if they 1) Show Improvement or 2) Hit the Benchmark: Each CCO that either hit the 68% figure or did better than their baseline would earn their Incentive Bonus.