Behavioral Health Performance Measurement
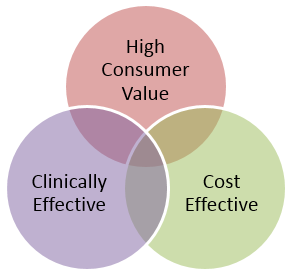
The Behavioral Health Performance Measurement System is the engine for measuring whether the care being provided is high-value, which is defined as patient centered, clinically effective, and cost effective care.
In order to measure value, stakeholders must agree upon and implement a set of performance measures that are most relevant to the three components of value and put in place a system of transparency and public reporting of results.
- Patient Centered: The care is easily accessible and provided by staff that communicate well, demonstrate knowledge and technical proficiency, and take enough time to address the needs of the client; (http://forces4quality.org/node/6805)
- Clinically Effective: The care is effective in achieving individual outcomes that matter to clients and system-wide outcomes that matter to payors and the community;
- Cost Effective: The care is more cost-effective than alternatives that may have been selected because of the treatment selected and/or because waste (excess costs) has been removed from the work processes.
In order to measure value, stakeholders must agree upon and implement a set of performance measures that are most relevant to the three components of value and put in place a system of transparency and public reporting of results.
Nationally, this behavioral health performance measurement work is occurring on two levels, which are explored in this toolkit: