Roadmap
This section of the toolkit focuses on reforming how RBHAs work with Providers reorganize and improve the system of care and payment structures to support the triple aim of better care, better health and better costs. Several of the nine steps described in the Roadmap are already underway at each RBHA, with preparation activities occurring in many of the provider organizations.
The most important purpose of the Roadmap (and toolkit in general) is to help RBHAs and Providers identify what they may have missed in their planning work and where they might be able to improve on work that is already underway.
Let’s explore each step on the Roadmap (pdf available here).
The most important purpose of the Roadmap (and toolkit in general) is to help RBHAs and Providers identify what they may have missed in their planning work and where they might be able to improve on work that is already underway.
Let’s explore each step on the Roadmap (pdf available here).
Step 1: Organize the Redesign Effort
Succeeding at Payment Reform Payment
Reform efforts have a much greater chance of succeeding when they meet the following criteria:
Reform efforts have a much greater chance of succeeding when they meet the following criteria:
- The project is guided by a set of Payment Reform Vision and Principles (Click here for an example of Behavioral Health Payment Reform Vision and Principles.)
- A Payment Reform Project Plan is created, followed, and adjusted as needed
- The Project Plan includes all of the Necessary Steps (The nine steps in this Roadmap are an example; click here to download a copy.)
- The project has a dedicated Project Manager (With adequate capacity and skills.)
- The process is Inclusive and Transparent (All stakeholders are included in meaningful ways through the process.)
- Best Practices are utilized at every step in the process. (Including the ideas in this Toolkit.)
Step 2: Service Delivery Redesign

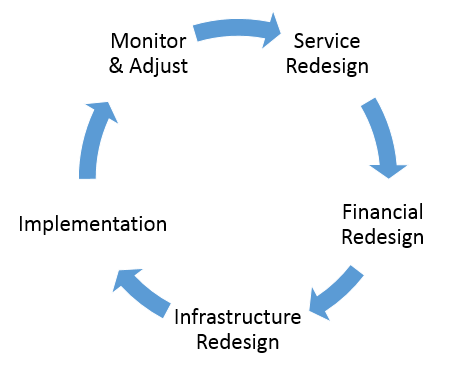
Many would argue that the U.S. healthcare system has higher costs and lower quality than peer countries because we have a ‘sub-optimized’ delivery system that is kept in place by antiquated funding and payment structures. Healthcare transformation works when a system begins with Service Delivery Redesign and then supports the implementation of the design with Financial Redesign (Payment Reforms) and Infrastructure Redesign. Payment Reform completed without Service Delivery Redesign DOES NOT WORK.
The Service Delivery Redesign section of this toolkit dives into the key Service Delivery Redesign issues that should be considered by systems serving Americans with behavioral health disorders.
The Service Delivery Redesign section of this toolkit dives into the key Service Delivery Redesign issues that should be considered by systems serving Americans with behavioral health disorders.
Step 3: Balance the Investment Portfolio

A RBHA’s budget should be viewed as a portfolio that will perform best if it is properly balanced. This approach requires completion of the following tasks.
Task 1: Define the Funding Pools that represent each major category of care. The diagram is an example of six Funding Pools: Acute Care Hospital (including Emergency), Medical Specialty, Pharmacy, Primary Care, Behavioral Health, and Other.
Task 2: Determine the Current Size of each Funding Pool. The data can be drawn from the entity’s financial statements, budget documents or an actuarial study. The diagram is an example of a portfolio that is out of balance; too much money is spent on ‘sick care’ resulting in underfunding of services that are critical to achieving the triple aim.
Task 3: Evaluate the Balance of the current Funding Pool Portfolio. Are resources allocated in a manner that support achieving the aims of better care, better health and better cost? Note that in many health systems serving individuals with behavioral health disorders, inadequate upstream care is resulting in high spending on hospital, medical specialty, emergency room and diagnostic imaging services.
Task 4: Rebalance the Portfolio following the theory of change, as needed. This can be accomplished by researching best in class systems throughout the U.S., especially in communities where health reform is well underway.
Task 5: Develop a Multi-Year Transformation Plan made up of service delivery redesign strategies, payment reforms, and infrastructure development to move from the as-is state to the to-be state.
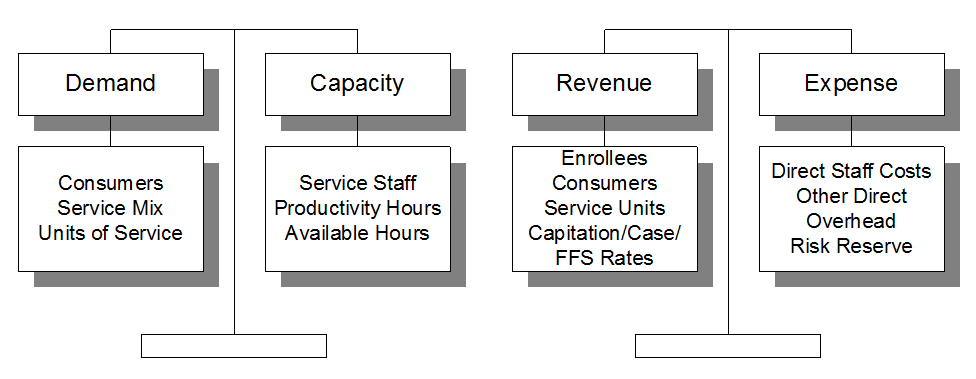
Task 6: Combine Tasks 1-5 into a Multi-Year Budget that balances demand with capacity and revenue with expense.
This work is essential for setting the direction of where service delivery improvements and payment reforms should be prioritized.
Utilization-Financial Modeling Tools
The Resources section of this toolkit contains useful material to support the Utilization-Financial Modeling activities. They include:
Task 1: Define the Funding Pools that represent each major category of care. The diagram is an example of six Funding Pools: Acute Care Hospital (including Emergency), Medical Specialty, Pharmacy, Primary Care, Behavioral Health, and Other.
Task 2: Determine the Current Size of each Funding Pool. The data can be drawn from the entity’s financial statements, budget documents or an actuarial study. The diagram is an example of a portfolio that is out of balance; too much money is spent on ‘sick care’ resulting in underfunding of services that are critical to achieving the triple aim.
Task 3: Evaluate the Balance of the current Funding Pool Portfolio. Are resources allocated in a manner that support achieving the aims of better care, better health and better cost? Note that in many health systems serving individuals with behavioral health disorders, inadequate upstream care is resulting in high spending on hospital, medical specialty, emergency room and diagnostic imaging services.
Task 4: Rebalance the Portfolio following the theory of change, as needed. This can be accomplished by researching best in class systems throughout the U.S., especially in communities where health reform is well underway.
Task 5: Develop a Multi-Year Transformation Plan made up of service delivery redesign strategies, payment reforms, and infrastructure development to move from the as-is state to the to-be state.
Task 6: Combine Tasks 1-5 into a Multi-Year Budget that balances demand with capacity and revenue with expense.
This work is essential for setting the direction of where service delivery improvements and payment reforms should be prioritized.
Utilization-Financial Modeling Tools
The Resources section of this toolkit contains useful material to support the Utilization-Financial Modeling activities. They include:
Step 4: Performance Measures
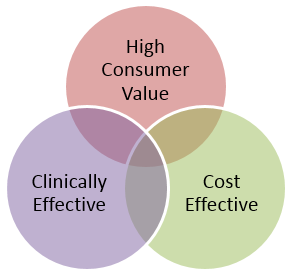
The Behavioral Health Performance Measurement System is the engine for measuring whether the care being provided is high-value, which is defined as patient centered, clinically effective, and cost effective care.
Patient Centered: The care is easily accessible and provided by staff that communicate well, demonstrate knowledge and technical proficiency, and take enough time to address the needs of the client; (http://forces4quality.org/node/6805)
Clinically Effective: The care is effective in achieving individual outcomes that matter to clients and system-wide outcomes that matter to payors and the community;
Cost Effective: The care is more cost-effective than alternatives that may have been selected because of the treatment selected and/or because waste (excess costs) has been removed from the work processes.
In order to measure value, stakeholders must agree upon and implement a set of performance measures that are most relevant to the three components of value and put in place a system of transparency and public reporting of results.
How to develop a Performance Measurement System is described in detail in the Measurement section of this toolkit.
Patient Centered: The care is easily accessible and provided by staff that communicate well, demonstrate knowledge and technical proficiency, and take enough time to address the needs of the client; (http://forces4quality.org/node/6805)
Clinically Effective: The care is effective in achieving individual outcomes that matter to clients and system-wide outcomes that matter to payors and the community;
Cost Effective: The care is more cost-effective than alternatives that may have been selected because of the treatment selected and/or because waste (excess costs) has been removed from the work processes.
In order to measure value, stakeholders must agree upon and implement a set of performance measures that are most relevant to the three components of value and put in place a system of transparency and public reporting of results.
How to develop a Performance Measurement System is described in detail in the Measurement section of this toolkit.
Step 5: Accountable Payment Models

In all healthcare systems, the Payment Model is the method by which Dollars and four types of Risk and Reward are transferred from the Payor to the Provider. We have identified four Payment Models that can be used for Behavioral Health Value-Based Purchasing:
These payment models and how to implement them are described in detail in the Payment Reform section of this toolkit.
- Capacity-Funded
- Modified Fee for Service
- Case Rate/Bundled Payment
- Sub-Capitation
These payment models and how to implement them are described in detail in the Payment Reform section of this toolkit.
Step 6: Pay for Performance/Pay for Success

It’s important to note that each of the four Payment Models described in Step 4 should be accompanied by a Pay for Performance (P4P) layer to ensure adequate provider accountability for cost and quality. It’s also important to consider a Pay for Success layer, which is a variation on P4P that is worth calling out.
Thus, it’s more accurate to label the four Accountable Payment Models that can be used for Behavioral Health Value-Based Purchasing as follows:
Thus, it’s more accurate to label the four Accountable Payment Models that can be used for Behavioral Health Value-Based Purchasing as follows:
- Capacity-Funded + P4P
- Modified Fee for Service + P4P
- Case Rate/Bundled Payment + P4P
- Sub-Capitation + P4P
Step 7: Infrastructure Development

The transformation and payment reform activities described in steps 2-6 represent a new way of doing business. And with that new business model comes the need to ‘remodel’ the RBHA and provider infrastructure to align with new business rules. The major areas are summarized below.
Information Technology: Most health plan and provider technology platforms do not support the integration of data across provider organizations to support integrated care, population health, robust tracking of outcomes and performance measures, and claims and billing models that stray from fee for service. This is the major Achilles Heel of transformation and payment reform.
Practice Guidelines: There is emerging agreement that ensuring that individuals receive the right care in the right setting in the right dosage requires a clear set of agreed-upon guidelines so that an individual who was mystery shopping, presenting with the same conditions at different organizations, would receive similar recommendations for the type of care that would be most helpful in helping them achieve their goals. This generally requires a Level of Care System, Utilization Management Structures, and a Best-Practices Toolkit.
Outcomes-Based Care Framework: The RBHAs and providers need to fully implement the type of outcomes-based care framework described in the Measurement section of this toolkit. This includes systems, tools and processes to measure and achieve systemwide outcomes and outcomes at the individual client level.
Reporting and Decision Support Platform: Value-added data that resides at various points in the system must be extracted, transformed and loaded into a robust data platform and then pushed back out in a variety of ways for a variety of purposes in formats that will enable decision making to support improvement at the individual level, demographic group level, and system level. It is also necessary to ensure transparency and public reporting of key information, while protecting patient/client privacy and confidentiality.
Workforce Development: RBHAs and providers understand that yesterday’s and today’s workforce has significant shortages in key areas and employees have been trained and are experienced in yesterday’s and today’s way of doing business. Identifying skill and knowledge gaps and rolling out training, supervision and coaching programs is as important for success has finding skilled workers to close the demand-capacity gaps.
Regulatory Barriers: Effective government is an accelerator of innovation; ineffective government creates barriers to innovation. One component of this project involved identifying regulatory barriers that will stymie or suboptimize the transformation and payment reform plan. Concerted effort must be made to systematically address these barriers, beginning with policies and regulations that are within the span of control of the RBHAs and providers and then working closely with AHCCCS, DBHS and, when needed, the Arizona Legislature to bring about regulatory relief.
Transformation Engine Development: There is a growing body of research that helps us understand that facilitating transformation involves a discrete set of knowledge, skills, processes, and tools, separate from what is required to ‘keep the trains running on time.’ These transformation components, combined with dedicated staff at the RBHA and provider levels make up the Transformation Engine. This is a critical part of infrastructure development that must be funded and brought online in order to realize promise of the new RBHA experiment.
Information Technology: Most health plan and provider technology platforms do not support the integration of data across provider organizations to support integrated care, population health, robust tracking of outcomes and performance measures, and claims and billing models that stray from fee for service. This is the major Achilles Heel of transformation and payment reform.
Practice Guidelines: There is emerging agreement that ensuring that individuals receive the right care in the right setting in the right dosage requires a clear set of agreed-upon guidelines so that an individual who was mystery shopping, presenting with the same conditions at different organizations, would receive similar recommendations for the type of care that would be most helpful in helping them achieve their goals. This generally requires a Level of Care System, Utilization Management Structures, and a Best-Practices Toolkit.
Outcomes-Based Care Framework: The RBHAs and providers need to fully implement the type of outcomes-based care framework described in the Measurement section of this toolkit. This includes systems, tools and processes to measure and achieve systemwide outcomes and outcomes at the individual client level.
Reporting and Decision Support Platform: Value-added data that resides at various points in the system must be extracted, transformed and loaded into a robust data platform and then pushed back out in a variety of ways for a variety of purposes in formats that will enable decision making to support improvement at the individual level, demographic group level, and system level. It is also necessary to ensure transparency and public reporting of key information, while protecting patient/client privacy and confidentiality.
Workforce Development: RBHAs and providers understand that yesterday’s and today’s workforce has significant shortages in key areas and employees have been trained and are experienced in yesterday’s and today’s way of doing business. Identifying skill and knowledge gaps and rolling out training, supervision and coaching programs is as important for success has finding skilled workers to close the demand-capacity gaps.
Regulatory Barriers: Effective government is an accelerator of innovation; ineffective government creates barriers to innovation. One component of this project involved identifying regulatory barriers that will stymie or suboptimize the transformation and payment reform plan. Concerted effort must be made to systematically address these barriers, beginning with policies and regulations that are within the span of control of the RBHAs and providers and then working closely with AHCCCS, DBHS and, when needed, the Arizona Legislature to bring about regulatory relief.
Transformation Engine Development: There is a growing body of research that helps us understand that facilitating transformation involves a discrete set of knowledge, skills, processes, and tools, separate from what is required to ‘keep the trains running on time.’ These transformation components, combined with dedicated staff at the RBHA and provider levels make up the Transformation Engine. This is a critical part of infrastructure development that must be funded and brought online in order to realize promise of the new RBHA experiment.
Step 8: Stress Test

A best practice that is used in many industries, but infrequently in the service sector, is to stress test a new design to assess how it might hold up under ‘real life’ conditions. Picture a Consumer Reports or General Motors laboratory stress testing a product or component of a product to see if stands up to heat, wear and tear, unanticipated jolts, etc.
Similarly, a Payment Reform initiative needs to use similar methods to determine how the initiative will stand up to real life circumstances. This includes three activities:
Similarly, a Payment Reform initiative needs to use similar methods to determine how the initiative will stand up to real life circumstances. This includes three activities:
|
Computer Modeling to test multiple demand/capacity and revenue/expense scenarios for balance.
|
Self-Assessment Tools at the RBHA and Provider levels to ‘search out’ gaps that may occur when new ways of doing business are rolled out.
|
Stress Test Work Sessions that include the following activities:
|
When used together, these three activities have the potential to significantly increase the probability of success and reduce the likelihood of potential failure points resulting in system failure.
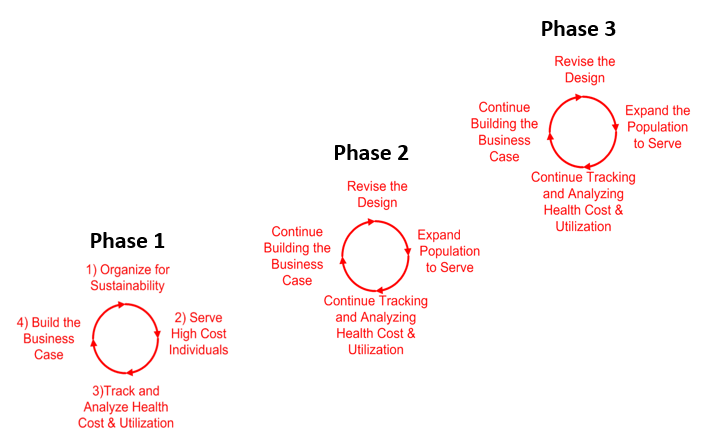
Step 9: Implementation Planning
Step 9 completes the cycle. When the design work that was planned in Step 1: Organize the Redesign Effort, is well underway, the RBHAs and providers will each need to build on their original project plans to create multi-phase Implementation Plans that are grounded in the Payment Reform Vision and Principles, breaks the work into realistic chunks (Phase 1, Phase 2, Phase 3), and continues to utilize dedicated Project Managers, working within the Transformation Engine, using Plan/Do/Study/Act cycles to roll out the necessary change initiatives.